Clinical trial safety profile
Adverse reactions in ≥5% of ARIKAYCE-treated patients with MAC lung disease (n=223) and more frequent than multidrug therapy alone (n=112) in the CONVERT trial1


| Adverse reaction | ARIKAYCE + multidrug therapy (n=223) n (%) | multidrug therapy alone (n=112) n (%) |
|---|---|---|
| Dysphonia a | 106 (48) | 2 (2) |
| Cough b | 88 (40) | 19 (17) |
| Bronchospasm c | 64 (29) | 12 (11) |
| Hemoptysis | 41 (18) | 15 (13) |
| Musculoskeletal pain d | 40 (18) | 10 (9) |
| Upper airway irritation e | 39 (18) | 2 (2) |
| Ototoxicity f | 38 (17) | 11 (10) |
| Fatigue and asthenia | 36 (16) | 11 (10) |
| Exacerbation of underlying pulmonary disease g | 34 (15) | 11 (10) |
| Diarrhea | 28 (13) | 5 (5) |
| Nausea | 26 (12) | 4 (4) |
| Headache | 22 (10) | 5 (5) |
| Pneumoniah | 20 (9) | 10 (9) |
| Pyrexia | 17 (8) | 5 (5) |
| Weight decreased | 16 (7) | 1 (1) |
| Vomiting i | 15 (7) | 4 (4) |
| Rash j | 14 (6) | 1 (1) |
| Change in sputum k | 13 (6) | 1 (1) |
| Chest discomfort | 12 (5) | 3 (3) |

No new safety signals detected2,3
In the open-label safety extension study of the CONVERT trial, the safety and tolerability of ARIKAYCE + multidrug therapy remained consistent.
No new safety signals were detected with up to 20 months of total ARIKAYCE exposure.
Respiratory AEs following ARIKAYCE initiation were common. Nephrotoxicity-related AEs and measured hearing decline were infrequent over the 12-month treatment phase in the extension study.
INS-312 was a 12-month open-label extension of the CONVERT trial that assessed the long-term safety and tolerability of once-daily ARIKAYCE + multidrug therapy. Eligible patients who completed both Month 6 and Month 8/EOT visits could consent to enroll directly in INS-312, in which case the Month 8/EOT visit served as the INS-312 baseline. All patients were treated with ARIKAYCE in INS-312. The frequency of TEAEs, TEAEs leading to study withdrawal, serious TEAEs, TEAEs of special interest, and clinically significant abnormalities in laboratory results and vital signs constituted the primary endpoint.
Additional adverse reactions in <5% of patients1
Selected adverse reactions that occurred in <5% of patients and at a higher frequency in ARIKAYCE-treated patients in the CONVERT trial included:
- Anxietyl (5% vs 0%)
- Oral fungal infectionm (4% vs 2%)
- Bronchitis (4% vs 3%)
- Dysgeusia (3% vs 0%)
- Hypersensitivity pneumonitisn (3% vs 0%)
- Dry mouth (3% vs 0%)
- Epistaxis (3% vs 1%)
- Respiratory failureo (3% vs 2%)
- Pneumothoraxp (2% vs 1%)
- Exercise tolerance decreased (1% vs 0%)
- Balance disorder (1% vs 0%)
- Neuromuscular disorderq (1% vs 0%)
The onset of new treatment-emergent adverse events (TEAEs) was most commonly reported in the first month of treatment4
TEAEs reported in ≥10% of patients receiving ARIKAYCE + multidrug therapy or multidrug therapy alone4


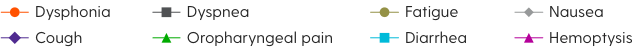
Data indicate the month at which the events were first reported after initiation of therapy.4
Adapted with permission of the American Thoracic Society. Copyright © 2023 American Thoracic Society. All rights reserved. The American Journal of Respiratory and Critical Care Medicine is an official journal of the American Thoracic Society. Readers are encouraged to read the entire article for the correct context at https://www.atsjournals.org/doi/pdf/10.1164/rccm.201807-1318OC. The authors, editors, and the American Thoracic Society are not responsible for errors or omissions in adaptations.
Incidence of TEAEs Month 1 to Month 6
- Patients who reported TEAEs and serious TEAEs in the CONVERT trial were 98.2% and 19.7% for ARIKAYCE + multidrug therapy vs 91.1% and 16.1% for multidrug therapy alone, respectively1,4
Discontinuations due to TEAEs primarily occurred early in the trial and declined over time.5
AE=adverse event; EOT=end of treatment; TEAE=treatment-emergent adverse event.
Implementing management techniques for respiratory AEs may be helpful for patients taking ARIKAYCE1,6
ARIKAYCE Prescribing Information1
Bronchodilator use
Consider using a short-acting bronchodilator prior to ARIKAYCE in patients with a history of reactive airway disease, asthma, or bronchospasm.
Findings from an ARIKAYCE management strategy survey (N=26)6
Lozenges
Soothing fluid intake
Changing ARIKAYCE administration to evening
Consider these techniques to address increased coughing or dysphonia.
- This information is not included in the ARIKAYCE Prescribing Information
- The data are from a telephone survey of 26 patients prescribed ARIKAYCE conducted during a 2-month period at 2 academic medical centers in the United States
- Writing assistance was provided to the authors through funding from Insmed. Insmed was not involved with the conceptualization, development, conduct, or analyses of the survey

